Introduction
Let’s talk about something that’s becoming a growing concern for healthcare practices —revenue cycle management. You will be surprised to know, recent revenue cycle management trends revealed that the denial rates have climbed to as high as 20% for both in-network and out-of-network claims. That’s a huge number, and it’s concerning healthcare practices. There is an urgent need for practices to rethink how they manage their financial processes.
The best solution to managing your financial process is leveraging revenue cycle management solution. It can address major financial issues like claim denials, delayed payments, and complicated regulatory compliance head-on.
Breaking Down the Healthcare Revenue Cycle Management Overview:
- Pre-Service Stage: This is where insurance verification happens, along with scheduling appointments. Think of it as laying the groundwork for smooth operations.
- Service Stage: Here’s where the magic happens—actual medical care is delivered and documented using medical coding.
- Billing Stage: Once services are provided, claims are submitted electronically to insurers. Accuracy at this stage is crucial to avoid denials.
- Payment Stage: Payments are collected from both patients and insurers. Delays here can seriously impact your cash flow.
- Post-Payment Analysis: This final step involves reviewing financial performance and pinpointing areas for improvement to ensure long-term stability.
When all these stages are streamlined using advanced RCM solutions, you’re not just managing revenue—you’re optimizing it. Accurate identification, collection, and management of practice revenue become achievable goals.
In this blog, we’ll dive deeper into the challenges healthcare providers face in RCM, explore the benefits of streamlining the process, and highlight some top RCM solutions that can transform your financial operations. Ready to uncover actionable insights? Let’s get started!
Did You Know ?
According to one survey, 92% of healthcare leaders are using AI and leveraging advanced RCM automation. It reflects how important it is today to leverage technology to streamline financial outcomes for healthcare providers.
Challenges in Healthcare RCM

Operational Inefficiencies
You know how frustrating it is when manual processing, disconnected systems, and duplicate data entry slow down everything. These operational inefficiencies waste your staff’s time and lead to errors, resulting in claim denials and delayed payments.
Imagine what if you cut down on those repetitive manual tasks with automated systems. That’s where revenue cycle management solutions come in to bring efficiency and accuracy to the table.
Claim Denials
The biggest headache for your practice is claim denials. Fixing and resubmitting the claims takes a lot of time, which eats up your staff’s valuable time and costs your practice millions per year.
But what if there was an automated tool that could run real-time eligibility checks accurately and submit claims to reduce denial rates? Sounds cool, right? This approach will save your staff from burnout due to manual error fixing and juggling with data and lower claim denial rates.
Delayed Payments
Slow payment cycles strain your cash flow. When patients or payers delay payments, you feel stuck in a financial bottleneck. Modern RCM systems are game-changers here—they speed up payment cycles with automated follow-ups, streamlined billing, and even patient-friendly payment options. It’s all about stabilizing your finances while making life easier for everyone involved.
Regulatory Compliance
Healthcare practices face a major challenge in complying with industry standards like HIPAA and changes in regulations that occur periodically. Failure to comply can result in major risk of losing your practice’s reputation and patients’ trust and facing hefty penalties.
All of these will ruin your practice reputation and impact revenue due to lost leads. Advanced RCM solutions can be of great help here, helping you comply with HIPAA and other regulations, avoid penalties and audits, and stay on top of industry rules.
Benefits of RCM You Should Know
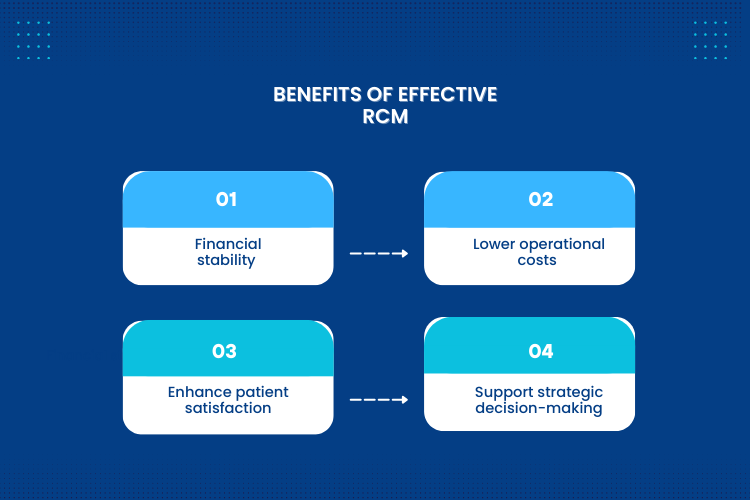
Financial Stability
You want to have a stable revenue stream. Effective healthcare RCM improves your claim acceptance rate and reimbursement rate and cuts down on administrative costs. When your practice has financial stability, you can grow your practice – from expanding facilities to investing in new technology.
Reduced Costs
Revenue cycle management solutions are a great investment for your healthcare practice as they help practices save money. When you leverage automation, you can reduce administrative tasks and errors. You can also lower the cost of rework for claim submission and extend account receivable periods with RCM solutions.
Enhanced Patient Satisfaction
Data Driven Decision Making
Revenue cycle management solutions help practices to get deeper insights into their business operations. It helps you analyze trends in claim denial or payment delays; therefore, you can know areas of improvements and make data-driven decisions that help you optimize your financial operations.
For A Detailed Guide on What Is RCM, Its Challenges & Benefits, & How to Select a Right RCM, Read Our Blog: Revenue Cycle Management: Streamlining Payments and Improving Efficiency
Choosing the Right RCM Solution
Evaluating Business Needs
Transaction Volume and Complexity
When you select healthcare RCM solution, you must consider their transaction volume and complexity. Large healthcare practices with diverse service lines require robust RCM solutions that can manage high volumes of complex claims, while smaller practices might require focused solutions with few functionalities. Understanding the scale and nature of financial transactions is crucial when searching for the right RCM solution.
Patient Mix
Existing Systems
Compatibility with existing systems is what you need to consider next when choosing RCM solutions. Integration capabilities that facilitate the smooth connection of practice management systems, electronic health records, and other software are provided by the best revenue cycle management solution. This integration ensures smooth data flow and eliminates redundant data entry, improving efficiency and reducing errors.
Key Features to Look For
Automation

Modern revenue cycle management solutions must include automation features. Thus, search for features like payment posting, claim scrubbing, denial management, and automatic real-time insurance eligibility verification. These automated systems speed up the revenue cycle and cut down on operational inefficiencies, freeing up staff to work on more difficult jobs that need for human intervention.
Integration

Second, you need to look for the integration feature when evaluating RCM solutions. The integration feature allows seamless flow of data between EHR systems, PMS, and patient portals. This ensures cohesive workflow and prevents data silos. An integrated revenue cycle management solution provides a comprehensive view of both clinical and financial data, enabling more informed decision-making.
Data Analytics

Modern RCM solutions now require advanced analytics capabilities. Seek revenue cycle management solution that offers up-to-date information on important performance metrics including net collection percentages, days in accounts receivable, and denial rates. These analytics enhance data driven decision making by assisting in the identification of trends, the localization of problem areas, and the evaluation of the impacts of process improvements.
Compliance and Security

When selecting a revenue cycle management solution, compliance and security capabilities are non-negotiable due to the increasing frequency of healthcare data breaches. Therefore, ensure that the RCM solutions comply with HIPAA guidelines and have strong security features in place to safeguard private patients and financial data. Standard offerings for the solution should include regular security updates and compliance monitoring.
Also, Read Our Blog: 8 Tactics to Improve Healthcare Revenue Cycle Management
Top 10 Healthcare Revenue Cycle Management Companies in 2025
For medical practices of all sizes, CERTIFY Health is a top cloud-based revenue cycle management system. While it lowers administrative hassles and claim denials CERTIFY Health’s Revenue Cycle Management System is built for streamlining invoicing, claims processing, and payment collection.
CERTIFY Health guarantees smooth insurance verification, real-time claims tracking, and effective reimbursement through robust automation. It improves workflow efficiency by seamlessly integrating with PMS, EHR, and EMR systems.
With its customized features, sophisticated analytics, and many payment methods, the platform delivers total financial transparency. Explore CERTIFY Health, it is an easy-to-use, scalable solution that helps clinics maximize revenue while preserving compliance and cutting expenses.
Key Features:
- Patient Scheduling: CERTIFY Health’s patient scheduling software lets your patients book appointments 24×7 using their smartphone, reducing phone time, no-shows, and errors.
- Patient Registration & Intake: CERTIFY Health allows pre-registration, enabling collection of patient intake and insurance details with the help of digital forms, reduce errors and enhance efficiency.
- Check-in & Authentication: CERTIFY Health’s patient check-in software offers digital check-in capabilities, check-in via mobile, laptop, or kiosk-faculty, ensuring smooth check-ins and easy data collection.
- Insurance Verification: CERTIFY Health enables real-time eligibility checks to confirm active insurance coverage before services are rendered, early verification reduces chances of claim denials and delays.
- Patient Communication: Automated reminders contribute to a more efficient claims processing experience by reducing the number of missed appointments and increasing the completion of required forms.
- Payment Management: By decreasing the number of missed appointments and improving the completion of necessary forms, automated reminders help to make the claims processing experience more efficient.
- Seamless Integrations: Payment systems and electronic health records (EHR) can be integrated to enable smooth data exchange, reducing errors and administrative expenses.
Waystar is another leading revenue cycle management solution in 2025. This cloud-based solution is dedicated to improving healthcare payments and enhancing financial performance for healthcare practices.
Waystar uses AI and automation to streamline processes, improve patient and provider experience, and reduce administrative burdens.
Key Features
- Eligibility Verification: This platform offers practice insurance eligibility verification capabilities to determine patient insurance coverage and prevent claim denials.
- Claim Management: This solution allows you to efficiently handle and submit the necessary data for claims processing and monitor and resolve claims issues promptly.
- Payment Management: This platform simplifies billing and helps you track and reconcile insurer payments. Not just that, patients offer various payment methods to ensure easy collections.
- Compliance: This platform adheres to regulatory compliance and ensures your practice and patients’ data is handled with care and is safe and secure.
Athenahealth is a revenue cycle management solution in 2025 designed for healthcare practices of all sizes. It aims to lower operational inefficiencies, help you get reimbursed faster, and improve healthcare revenue through automation.
When integrating advanced automation and interoperability, your practice can address various revenue cycle challenges and ensure optimal performance of your practice.
Key Features:
- Low-Touch Automation: It allows you to automate routine accounts receivable tasks, freeing your staff to focus on more complex tasks.
- Integration: This platform seamlessly integrates with your existing systems, such as EHRs, EMRs, etc., to facilitate smooth data exchange and improve workflow and team collaboration.
- Registration: Collect necessary patient details during registration; accurate information ensures a seamless process.
- Insurance Verification: Athenahealth enables real-time insurance verification and co-pay identification, improving collections and claims submissions.
- Accurate Billing: This solution collects accurate patient information, helping you code properly and reducing medical billing errors. You can also automate payment reconciliation to ensure accurate financial records.
R1 RCM is a technology enables revenue cycle management solution, designed to transform your practice’s financial performance. It leverages artificial intelligence (AI), automation, and deep data analytics to optimize healthcare revenue cycles, achieving optimal financial performance while maintaining delivery of exceptional patient care.
Key Features:
- Patient Registration & Financial Clearance: easy and accurate patient data collection, insurance verification and financial responsibility estimation before service delivery, minimize errors and reduce claim denials.
- Pre-Authorization & Eligibility Verification: Automates the insurance verification process and prior authorizations to reduce delays and ensure smooth claim approvals.
- Claims Management & Submission: Streamline your insurance claims processing with automation, validate claims before submission, reducing risk of rejections.
- Denial Prevention & Revenue Recovery: Make use of predictive analytics to identify pattern of claim denials and recover lost revenue from previously denied claims.
- Patient Billing & Payment Solutions: Offers user-friendly payment options to your patients, send automated reminders, and offer flexible payment plans to ensure easy collections and improve patient satisfaction.
TruBridge is another well-known tech-enabled revenue cycle management solution in 2025. It offers a comprehensive solution that streamlines your revenue cycle process, reduces administrative costs, and ensures quality care delivery – all at the same time. Their solution is customizable meaning – it can fit the needs of healthcare practices no matter if it is a small practice or large healthcare organizations.
Key Features:
- Electronic Health Record Solutions: This platform centralizes medical, financial, and administrative functions, giving access to patient records, billing, and insurance information while minimizing workload and inefficiencies.
- End-to-End RCM system: this solution is designed to automate and optimize your RCM for financial stability of your practice. Streamlining the entire process from registration to insurance verification, billing to payment collections.
- Revenue cycle disruption: TruBridge enables you to automate follow-ups and claims resubmissions to ensure faster reimbursement and identify issues in cash-flow.
- Medical Coding: TruBridge enhances the accuracy of claim submissions by ensuring correct coding. Accurate medical service coding lowers the possibility of claim delays and denials, resulting in faster payouts.
- Patient Billing & Payment Solutions: With the use of their AI-powered analytics tool, you may find operational inefficiencies, obtain a comprehensive picture of revenue cycles, and make data-driven financial decisions for enhancements.
FinThrive is sixth in our list of top revenue cycle management solutions in 2025. It offers a comprehensive approach to financial operations and addresses operational inefficiencies through intelligent work routing and workflow automation.
Key Features:
- Patient registration: This platform makes the patient registration process much easier, the digital forms ensure accurate patient details are collected and validated, avoiding manual errors and reducing staff burnouts.
- Remote Check-in: Your patients can complete the check-in process online and any documents (patient intake) before entering the medical facility, increasing convenience and decreasing front-desk congestion.
- Claims Manager: Using this platform, you can automate the claims submission process, reduce errors, and speed up the reimbursement process.
- Eligibility Verification: To increase revenue collections, instantly confirm the billable insurance coverage, co-pays, and deductibles.
- FinThrive Analyze: You can use advanced data analysis with this feature, which provides an enterprise-wide view for quick gap detection and more informed decision-making.
DrChrono’s revenue cycle management solution is a cloud-based platform that comes with EHR, medical billing, and practice management capabilities. It has easy to use user interface and offers mobile accessibility. DrChrono helps healthcare practices streamline revenue cycle management, reduce administrative inefficiencies, and improve financial stability.
Key Features:
- Billing Management: DrChrono’s billing management solution handles everything from accurate patient eligibility verification to medical billing, denial follow-ups, and payment collections.
- Scheduling: It offers features like appointment booking, automated reminders, and customizable patient flags to ensure scheduling efficiency and effective communication.
- Payment Collections: It helps you to make the collection process hassle-free by sending statements or bills online to your patients, ensuring easy collection of payment bills.
- Mobile Accessibility: Their solution is cloud-based and available to access on iPhone, iPad, or the web, ensuring practice has the convenience to manage practice-on-the-go.
MD Clarity is designed to ensure transparency and efficiency in healthcare payments through effective revenue cycle management. This platform will help you reduce claim denials and maximize collections of payments. It easily integrates with your EHR system or PMS to ensure workflow optimization and reduce operational inefficiencies.
Key Features:
- Cost Estimates: MD Clarity helps practices ensuring financial transparency with their patients through real-time cost estimates, this avoids surprises and allows upfront payment collections.
- Customizable Scheduling: It helps by enabling your patients to book appointments online, reduce no-shows, send automated patient notification, and offer an easy rescheduling option.
- Seamless EHR & PMS Integration: With EHR and PMS integration capabilities, data can be synced in real-time across the platforms, helps in maintaining up-to-date records and reducing front-desk manual overload.
- Automated Claim: This feature enables proactive claim scrubbing, ensuring compliance checks and reducing claim denials through issue identification and correction.
Change Healthcare (now part of Optum) is another robust revenue cycle management solution in the market. This platform offers comprehensive ARCM capabilities, from advanced claims processing to revenue integrity tools. Their solution addresses RCM challenges like high transaction volumes with its high throughput processing capabilities.
Key Features:
- Scheduling & Patient Registration: This software simplifies scheduling and registration process, sends automated reminders to reduce no-shows, and enables pre-registration to collect patient details accurately.
- Insurance Verification: The platform provides real-time eligibility and benefits verification to minimize coverage-related claim denials.
- Medical Coding & Charge Capture: Medical coding powered by AI improves accuracy and compliance while lowering claim errors. Automatic charge capture guarantees that no money is lost, and integrated validation tools support the accuracy of the coding.
- Billing & Payment Processing: The system creates electronic billing statements and offers various payment options to speed up collections. Automated payment reminders for unpaid invoices assist healthcare providers in sustaining a steady cash flow.
- Analytics & Reporting: The system provides real-time insights into financial performance via customizable dashboards. Predictive analytics facilitate revenue forecasting, enabling healthcare providers to make informed financial decisions.
Medsphere RCM Cloud completes the list of our top 10 healthcare revenue cycle management companies for 2025. This is a cloud-based platform that comes with easy deployment and scalable pricing structures, making it suitable for healthcare practices of varying sizes. Medsphere’s solution features robust integration capabilities with current systems, facilitating seamless data exchange and maintaining workflow continuity.
Key Features:
- Patient Scheduling: The Medsphere RCM Cloud allows you to manage appointments and optimize patient flow, reducing scheduling hassles and wait-times.
- Patient Registration: This platform offers digital patient registration to ensure easy and accurate data collection from your patients, reducing administrative burdens and inefficiencies.
- Insurance Verification: This platform enables you to automate insurance eligibility verification, you can verify insurance during registration or scheduling, ensuring early identification of coverage and timely claim submissions.
- Integration Capabilities: This platform seamlessly integrates with the EHR system to maintain easy access to updated patient information and smooth workflow.
- Billing and Claims Processing: Automates billing workflows and claim submissions to reduce errors and speed up reimbursement and payment collections.
Conclusion
Healthcare practices must now concentrate on investing in a revenue cycle management solution that can lower claim denials, a major difficulty in RCM, and satisfy regulatory requirements because the healthcare financial landscape is complicated and always changing.
It is worthwhile to investigate the revenue cycle management solutions discussed in this blog in order to reduce claim denials, expedite payment collection, and minimize operational inefficiencies such as incomplete or erroneous insurance eligibility verification.
Healthcare providers should thoroughly assess their business needs, including transaction volume, patient mix, and current systems, to ensure that they are choosing the best solution.
Exploring demos of the top RCM solutions mentioned above is a practical next step for healthcare organizations ready to transform their financial operations.