Introduction
Did you know that the goldfish has an attention span of only 9 seconds? But you will be more surprised to know that your patients have even less attention span when dealing with insurance complications.
Here’s what you need to do: master patient insurance eligibility verification in RCM. It can transform your healthcare practice’s financial health and patient satisfaction overnight.
What is RCM in healthcare? If I were to define revenue cycle management, it’s the entire financial journey of your patient’s care—from the moment they schedule an appointment until the final payment clears. That’s right, it’s not just billing—it’s the comprehensive financial heartbeat of your practice.
For healthcare organizations to maintain financial stability and continue providing quality patient care, effective RCM is essential. This includes charge capture, claim submission, coding, patient collections, registration, remittance processing, and eligibility verification in RCM.
Wait—did you know that 26.6% of claim denials come from eligibility issues? That’s right. Eligibility verification in RCM is not just about paperwork—it’s protection for your revenue stream
Since most Americans rely on health insurance, proper eligibility verification in RCM is imperative for practices seeking effective reimbursement and elimination of unpaid claims. By confirming patient insurance coverage upfront, you avoid the costly nightmare of denied claims and payment delays.
In this blog, we will look at the five actionable steps to integrate patient eligibility verification in RCM effectively.
You might also like to read: Revenue Cycle Management: Streamlining Payments and Improving Efficiency
5 Steps to Revolutionize Your RCM with Seamless Eligibility Verification
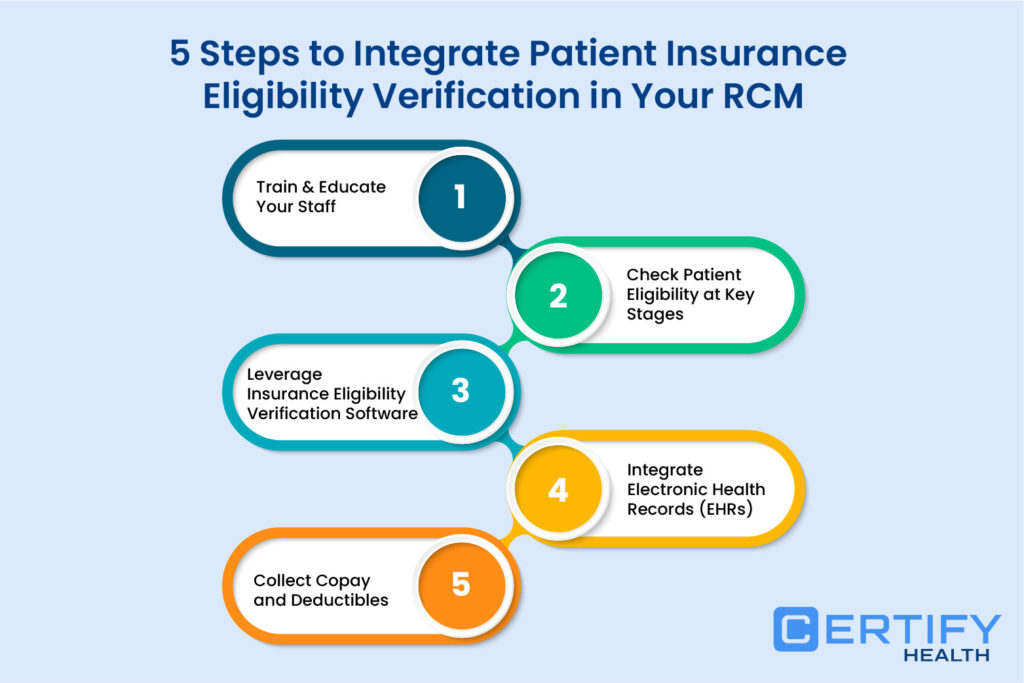
Staff training and education
Your staff is a great asset, but what if they are not trained well? (Ouch! That might lead to some costly mistakes.)
Inadequate staff training and education on eligibility verification can result in denied claims and delayed reimbursements. That’s why you must empower your team with skills to verify insurance in real time, reducing burnout, and errors. This will improve your financial outcomes and enhance patient satisfaction.
Tip
Tools like CERTIFY Health’s insurance verification software not only helps you verify insurance eligibility in real-time but also offer comprehensive training and 24/7 support to ensure your staff is always on top of their game.
Check Patient Eligibility at Key Stages
When was the last time you checked patient eligibility? If your answer is “at check-in only,” you are missing crucial opportunities to prevent denials.
Timing is everything when it comes to eligibility verification. Checking your patient eligibility at critical stages—scheduling, intake, and check-in—can prevent errors and denials before they happen.
When should you check patient eligibility? The optimal approach includes verification during:
- Appointment Scheduling: Collect & verify insurance details on the first content while scheduling
- Pre-registration: Verifying coverage details 2-3 days before appointment
- Patient Intake: Confirming insurance information during paperwork completion
- Check-in: Final verification immediately before service provision
Check patient eligibility at these critical junctures and watch your clean claims rate soar while denials plummet.
Tip
Modern solutions like CERTIFY Health make this seamless, integrating automated verification across your patient’s journey to ensure accuracy and efficiency.
Leverage Insurance Eligibility Verification Software
Let’s be honest—manual verification is like using a typewriter in the age of cloud computing.
It’s slow, error-prone, and just plain inefficient. Manual verification creates substantial time burdens, with staff spending precious minutes on tasks that could be automated in seconds.
The benefits of automation extend far beyond time savings—it improves clean claim rates, reduces those frustrating denials, and accelerates your entire revenue cycle.
The benefits of automation make eligibility verification in RCM practically effortless, integrating seamlessly with your existing systems for a unified approach to financial management.
Tip
With automated verification solutions like CERTIFY Health, you can automate eligibility checks, freeing your staff to focus on what matters—patient care.
You might also like to read: 5 Expert Tips to Achieve 100% Accurate Patient Insurance Eligibility Verification
Integrate Electronic Health Records (EHRs)
Is your eligibility data trapped in a system that doesn’t talk to your EHR? That can create a recipe for confusion and errors for your teams.
Integrated EHR solutions ensure that eligibility verification in RCM doesn’t exist in a vacuum. By connecting these critical systems, you maintain data accuracy and eliminate confusion during claims processing.
Integrated EHR implementation facilitates better team collaboration by making all relevant information accessible in one place. This streamlined approach to eligibility verification in RCM ensures that everyone has the same, accurate information.
Integrated EHR systems update insurance information in real-time, ensuring that patient data is current and consistent across all touchpoints.
Tip
CERTIFY Health’s practice management solution makes this integration seamless, connecting with major EHR, practice management, and billing systems.
Collect copays and deductibles
Do you know what’s better than billing a patient after service? Collecting payment before they leave!
Collecting copays and deductibles from patients from patients at the time of service dramatically improves cash flow and reduces billing headaches. When you combine this with eligibility verification in RCM, you create a transparent financial experience that patients actually appreciate.
Collecting copays and deductibles from patients can be seamless when you have real-time eligibility information at your fingertips. This approach to eligibility verification in RCM ensures financial responsibilities are clear to patients upfront.
Collecting copays and deductibles from patients during scheduling, intake, or check-in prevents billing issues later on, improving overall patient satisfaction and practice revenue.
Conclusion
Still reading? Good – because eligibility verification in RCM is no longer optional for practices that want to thrive. It is imperative for your practice to understand what is revenue cycle management, the role of insurance eligibility verification in RCM and integrating it seamlessly.
Implementing these five steps will help you integrate patient insurance eligibility verification in RCM, dramatically reducing denials, accelerating payments, and making your revenue performance soar.
Explore the solutions like CERTIFY Health that can automate eligibility verification in RCM, integrate with your existing systems, and provide the real-time data needed for informed financial decisions. Book a personalized demo!