Introduction
You might have experienced it multiple times – your patients waiting in a packed room, staff busy on never-ending calls, nurses rushing past, and getting frustrated over a double-booked exam room.
On the other hand, your patients may get boiled up, three of them may just walk out without getting seen, or some appointments may be canceled at the last moment. Not only is this frustrating, but it can cost you thousands of dollars.
One study found that missed appointment rates in US healthcare range from 5.5 to 50%. This not only drains your staff’s time and resources but also impacts revenue cycle management.
But here’s the kicker: About 80% of these no-shows are preventable if you follow some patient scheduling best practices, it can help you with appointment management. Curious to know more? Then, keep reading.
In this guide, we have listed five patient scheduling best practices that transform your workflows while keeping HIPAA compliance, revenue growth, and patient satisfaction front and center.
Why Efficient Scheduling Isn’t Optional
Because inefficient scheduling is not just annoying but also expensive. Just imagine:
How much time do your staff spend weekly on manual appointment booking and reminder calls? This not only drains your staff’s time but leads to burnouts, increase employee turnover, and leave no time for patient care.
Also, think about how much unplanned patient no shows might cost your practice (billions annually). You have to look for effective scheduling methods to save both your staff from burnouts and prevent cost leakage.
Benefit: When done right? Patient scheduling can boost your patient experience, patient & staff retention, optimize resource allocation, and reduce operating costs efficiently.
Let’s discuss this in depth:
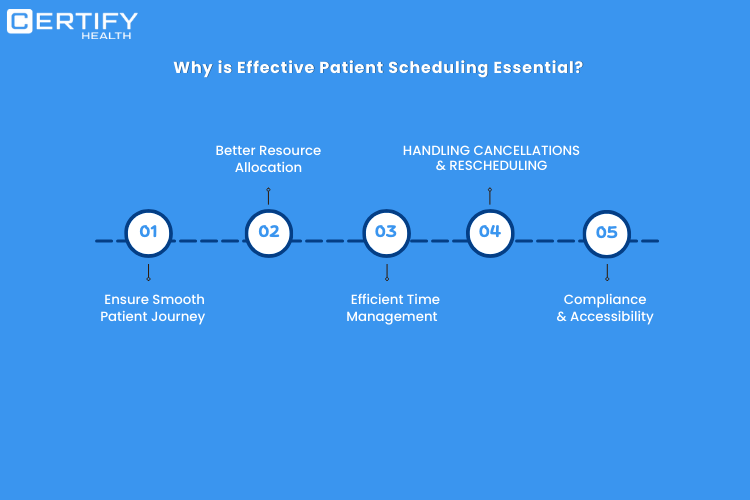
1. Smooth Patient Journey: First Impressions Matter
Appointment booking sets the tone for the entire healthcare experience. A clunky process—like forcing patients to call during limited hours—immediately erodes trust. Modern solutions? Patients can schedule, postpone, or cancel appointments at any time via patient self-scheduling portals.
Key stat: 43% of patients prefer booking their appointments after business hours as per a study. If you miss the window, you are leaving money on the table.
2. Resource Allocation: Work Smarter, Not Harder
Efficient scheduling is not about filling slots—it’s about resource allocation and that requires you to look for strategic solution. Think about this:
- Balanced workloads: Determine how many appointments your staff can handle in a day without compromising on care quality. Utilize digital tools for patient appointment management, distribute appointments evenly across staff, considering factors like skill level and availability.
- Room utilization: Categorize rooms based on their purpose (e.g., exam, procedure, consultation). Look how much time is needed for each type of appointment. Use software to assign rooms based on appointment length and type.
- Equipment readiness: Sync schedules with inventory systems to track the availability and maintenance of equipment. Conduct routine checks before appointments to confirm equipment is sterilized and functioning properly.
3. Efficient Time Management: The Art of Predictability
Ever had a routine physical derailed by an unexpected 90-minute delay? Buffer slots are your lifeline. By analyzing historical data, top practices:
- Accurately estimate appointment lengths (e.g., 15 mins for follow-ups vs. 45 mins for new patients).
- Build 10–15-minute cushions between visits to handle overruns.
- Automatically flag chronic latecomers for earlier time slots.
Result? Patient wait times will drop and practices will regain lost hours weekly previously spent apologizing for delay.
4. Efficient Time management: Stop the Bleeding
Last-minute appointment cancellations are a big headache, per cancelled appointment, you lose not just time but money as well which cannot be recovered. Efficient patient scheduling can solve this:
- Automated waitlists: Fill canceled slots by notifying patients on the waitlist and ASAP list for priority appointments.
- Appointment Cancellation fees: Enforce clear policies (e.g., “48-hour notice required”) to deter no-shows.
- Flexible rescheduling: Let patients self-adjust appointments via portal, reducing phone tag, enabling patients to pick appointment time as per their convenience.
Did you know?
An observational study found that patients who received SMS reminders had a no-show rate of 11.2%, compared to 18.1% in those who did not receive reminders. This represents a 38% reduction in missed appointments.
5. Compliance & Accessibility: Protect and Serve
Compliance is necessary and cannot be ignored. HIPAA compliance in patient scheduling involves protecting sensitive patient information while collecting details during scheduling. Mostly, protected health information (PHI) shared over call is at risk of breach.
So, use HIPAA-compliant scheduling software that can help you avoid data breach risk and adhere strictly to changing regulations. Patient scheduling software enables practices to control access (who can view your data) and limits access (who can edit your patient information).
Remember that compliance isn’t just about security, it is also about how you accommodate patient with special needs as well:
- Telehealth offerings: Offer video consultations to patients facing mobility issues (due to health concerns or are living in remote areas) or tight schedules.
- Extended hours: Use self-scheduling to accommodate night owls and early birds alike.
- Multilingual support: Automate reminders in the patient’s preferred language.
Also, Read our blog on: What is Patient Scheduling Software?
5 Patient Scheduling Best Practices to Implement Now
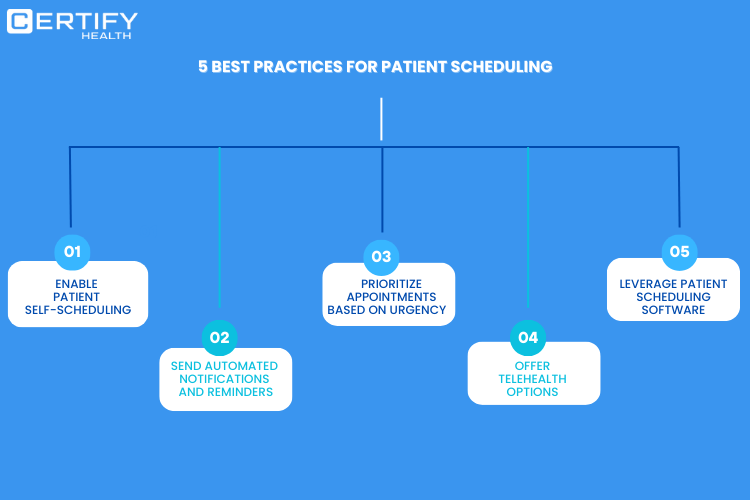
1. Ditch the Phone Tag: Enable Patient Self-Scheduling
Traditional scheduling methods – hours long phone calls – wait times – error prone. (You are aware that this will not work for you).
You need patient self-scheduling software like CERTIFY Health’s patient scheduling software that empowers patients to book online appointments, reduce wait times, and protect your staff from phone tags and burnouts.
Benefits?
- 24×7 accessibility to book, reschedule, or cancel.
- Real-time availability checks to prevent double-booking.
- Insurance verification during registration to reduce check-in delays.
- Intake form integration so patients’ complete paperwork pre-visit.
2. Automate Reminders: Nudge, Don’t Nag
As discussed earlier, missed appointments cost practices billions annually. That’s where automated reminders comes into the picture!
Say goodbye to no-shows, “hi” to appointment visits! Here’s all you need to do, use tool like CERTIFY health that offers feature like automated reminders to reduce patient no shows and automated notifications to engage patients on different interval of time like:
- 7 days before visit: “Your appointment is scheduled for
- 24 hours prior: “Reminder: Fasting required for tomorrow’s bloodwork.”
- 2 hours prior: “Dr. Lee is ready early! Arrive by 1:45 PM?”
Advanced systems even analyze patient behavior, like sending extra reminders to frequent no-shows.
3. Triage Urgent Cases Without Torpedoing Your Schedule
Urgent care needs can disrupt schedules if not managed strategically. Proper triage ensures critical cases are addressed promptly without throwing off the entire day’s workflow.
- Dynamic scheduling blocks: Reserve 10-20% of daily slots for urgent needs.
- AI-powered triage: Chatbots assess symptoms to route patients to same-day slots or telehealth.
- Provider load balancing: Automate urgent requests to the least-busy clinician.
4. Telehealth Offerings: The No-Show Killer
Telehealth bridges the gap between patient accessibility and provider availability, significantly reducing barriers like travel time or scheduling conflicts.
What it means?
- Eliminates travel: Best for rural or immunocompromised patients
- Fills last-minute gaps: A 10-min telehealth follow-up beats an empty slot.
- Boosts revenue: Charge copays for quick check-ins that used to be free phone calls.
- Pro move: Use automated post-visit surveys to identify patients who’d benefit from hybrid care.
5. Invest in HIPAA-Compliant Scheduling Software
Forget spreadsheets and paper calendars. Outdated methods like spreadsheets can lead to inefficiencies and compliance risks. Modern tools like CERTIFY Health offers HIPAA compliant patient scheduling, ensure secure, streamlined scheduling for you and your patients.
Benefits?
- Protects sensitive patient information (PHI) from unauthorized access & breaches.
- Reducing legal risks, costly fines, and reputational damage.
- Enables tracking of patient data access and modifications.
The Bottom Line: Better Scheduling = Healthier Bottom Lines
Patient scheduling isn’t about filling chairs—it’s about orchestrating a symphony of people, time, and technology. By adopting patient scheduling best practices, practices can:
- Slash no-show rates
- Save time & increase staff productivity
- Improve annual revenue via optimized capacity
So, what’s the next step? Start exploring top 10 patient scheduling software and choose the best solution that can help you manage scheduling and offer features to implement the above-mentioned best practices.